A stricter standard sounds healthier—but is it?
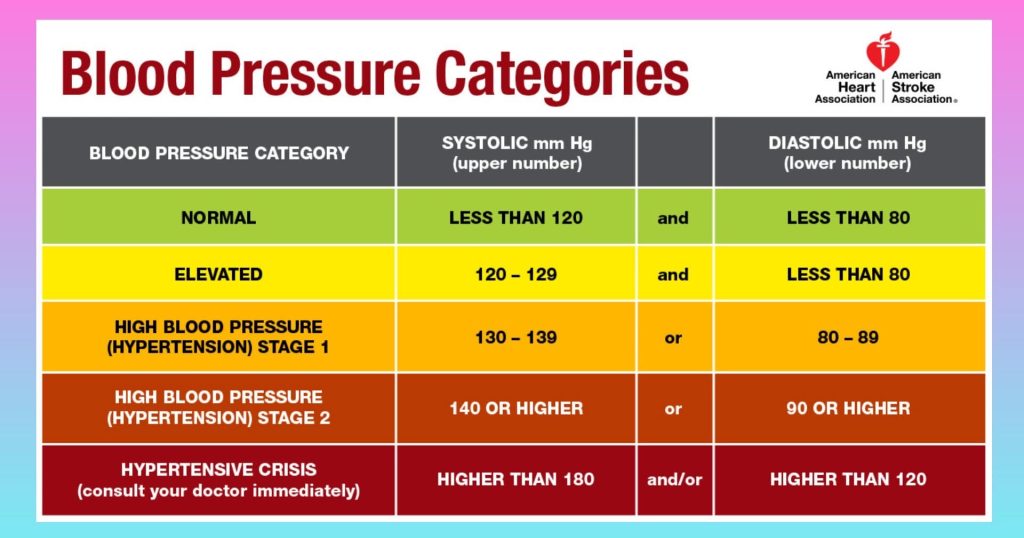
The American Heart Association (AHA) grabbed attention this week by redefining “normal” blood pressure as anything below 120/80 mm Hg. At first glance, the move seems like progress, a push toward better heart health. Yet behind the reassuring tone, millions of Americans could face brain fog, dizziness, and unnecessary prescriptions.
The new benchmark tightens the definition of healthy blood pressure, meaning that people who once felt confident about their numbers now fall into the “elevated” category. This shift, while well-intentioned, sets up a wave of new diagnoses and treatments that may do more harm than good.
Lower Numbers, Higher Risks
Physicians who supported the change said the data show early damage begins above 120. However, critics warn that aggressively lowering blood pressure can backfire. When medication pushes numbers too low, blood flow to the brain can drop, triggering confusion and chronic fatigue.
Dr. Robert A. Phillips, chief medical officer at Houston Methodist and a noted hypertension specialist, has found that intensive blood pressure treatment can harm lower-risk patients, sometimes outweighing the benefits of strict control. His research warns that stricter guidelines could trade one significant health condition for another, particularly through unnecessary diagnoses and aggressive interventions that create new risks for vulnerable groups.
In addition, reduced kidney perfusion, especially in older adults, can lead to dehydration and declining kidney function. Nephrologists have already raised alarms, pointing out that overmedication often lands patients in the hospital with preventable complications.
Big Pharma Gains, Patients Lose
With tighter standards, prescriptions will likely rise. Every patient whose pressure lands between 120 and 130 suddenly becomes “at risk,” giving physicians reason to prescribe additional drugs. Pharmaceutical companies benefit, but ordinary people bear the side effects—lightheadedness, electrolyte imbalances, and mounting costs.
At the same time, blood pressure medications rarely work in isolation. Patients taking multiple drugs for heart disease and cholesterol will face complex regimens that increase the chance of side effects and interactions.
The Data Debate
Cardiologists remain divided over whether chasing ultra-low numbers extends life. The AHA based its decision on a collection of studies showing fewer heart attacks in patients who maintained readings near 120. Yet many of those trials involved highly monitored hospital settings—not real life.
“Those studies don’t reflect what happens when a 70-year-old woman takes multiple medications at home,” said Dr. Elaine Torres, a Boston-based internal medicine specialist. She argues that what works in a study population can harm high-risk groups when applied broadly.
Health Through Simplicity, Not Strain
Instead of pushing people to lower their blood pressure at all costs, many experts urge a simpler message: move more, sleep better, eat whole foods, and manage stress. These behaviors naturally control pressure without the need for prescriptions or side effects.
By lowering what counts as “normal,” the AHA may unintentionally turn wellness into a medical condition. Millions who once viewed themselves as healthy could now live under new anxiety, tracking every number and pill.
A Misstep in the Name of Prevention
In its effort to prevent heart disease, the AHA may have crossed into overcorrection. While the association claims tighter control saves lives, the hidden consequences, brain fog, kidney damage, and medication dependence, deserve public attention. True health should mean freedom, not fear of a blood pressure reading that once seemed perfectly normal.
Dr. Franz Messerli, cardiologist at the University of Bern, also cautions that targeting systolic blood pressure below 120 for otherwise healthy adults is “absurd.” He contends that while stricter control may reduce stroke events for high-risk populations, evidence does not support aggressive treatment for many adults. Messerli highlights side effects such as dizziness, fainting, and increased medication burden as complications seen when blood pressure is lowered excessively, especially with multiple antihypertensive drugs.



