Irritable bowel syndrome (IBS) is recognized as the most prevalent gastrointestinal disorder worldwide, yet it remains underdiagnosed in many populations. The impact of IBS ranges from mild discomfort to significant disruption in daily living, but crucially, it does not lead to permanent intestinal damage or escalate into more serious diseases such as cancer.
Understanding Irritable Bowel Syndrome
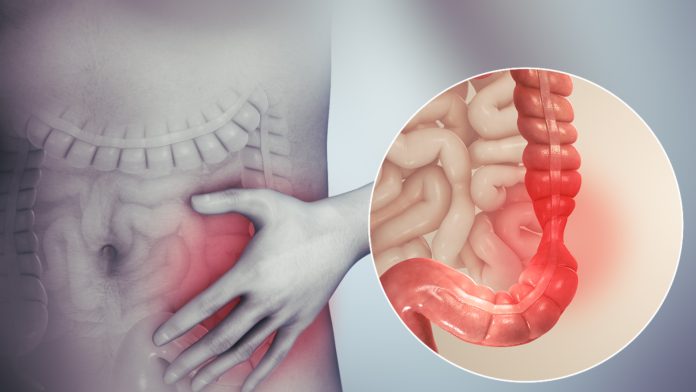
IBS is a chronic gastrointestinal disorder characterized by widespread symptoms and a variable course. It affects both the small and large intestines and is considered a functional condition, meaning it impacts the digestive system’s function without causing visible structural damage. The prevalence of IBS is notable, with up to 15 percent of adults in the United States experiencing symptoms at some point. Despite its frequency, less than half of these individuals receive a formal diagnosis, often due to the subtlety and overlap of symptoms with other disorders.
Key Symptoms to Monitor
IBS manifests in diverse ways, making recognition difficult. Abdominal pain or discomfort is consistently prominent and often eases after a bowel movement. Changes in bowel habits range from constipation and diarrhea to alternating episodes of both. Many sufferers experience bloating, a sensation of fullness, and increased flatulence, which reflects typical gastrointestinal difficulties. Additional reports include mucus in the stool and a persistent feeling of incomplete evacuation following restroom visits, alongside occasional nausea or even fatigue. These symptoms commonly fluctuate over time, intensifying during periods of stress or after consuming certain foods.
Triggers and Individual Management Strategies
Numerous factors influence the course of IBS. Foods such as caffeine, alcohol, and spicy meals are regular triggers, but emotional stress and anxiety can be equally significant in precipitating or worsening symptoms. Some patients notice a correlation between symptom flare-ups and the use of antibiotics. Effective management is often multimodal, incorporating dietary modifications, medication, and behavioral interventions like stress reduction or cognitive therapy. Careful attention to personal triggers and lifestyle adjustments typically yields positive outcomes, enabling patients to gain greater control over their condition.
When Expert Help Is Required
Although IBS in itself is not a cause of serious illness or mortality, specific symptoms must be carefully monitored. Medical guidance is essential if an individual experiences unexplained weight loss, blood in the stool, intense, persistent abdominal pain, or additional symptoms such as fatigue and pallor that may point to more significant underlying conditions. Timely consultation with healthcare professionals ensures appropriate evaluation and the exclusion of other diseases that may mimic IBS.
IBS is a widespread, yet often misunderstood, digestive disorder with the potential to impair the quality of life for millions. Understanding the spectrum of symptoms and their triggers is key in achieving an effective diagnosis and optimizing treatment strategies. With appropriate management, most individuals living with IBS find they can minimize disruptions and lead fulfilling lives.